Watch for These Bladder Warning Signs
Here on The OAB Clinic, your comprehensive patient information portal, we spend a lot of time talking about Overactive Bladder (OAB) treatments that you can manage on your own. My goal is to make your journey to finding your better bladder as easy as possible. However, there are some bladder situations that should prompt an evaluation by a health care provider, possibly even one who specializes in Bladder and Pelvic Health.
Should I worry if I have Overactive Bladder symptoms?
Most people with symptoms of Overactive Bladder (OAB) such as frequent or urgent urination do not require extensive or invasive evaluation. In fact, the guidelines of the American Urological Association for OAB discourage the use of this kind of testing early on in the evaluation of uncomplicated OAB. However, you should be aware that certain symptoms increase the possibility of a more serious condition. These bladder warning signs suggest the need for a more thorough and complete evaluation than you can accomplish on your own. They may even prompt you to see a bladder health specialist, such as a urologist specializing in Pelvic Health. For instance, sudden onset of symptoms, especially if accompanied by pain (which is not a symptom of OAB), often indicates another problem such as an infection or a urinary tract stone. Blood that you see mixed into your urine is also not a symptom of Overactive Bladder and should be investigated by a urologist.
What are other warning signs that my Overactive Bladder symptoms should be looked at more closely?
In addition to blood in the urine and pain, there are several additional warning signs that you may need to see a urologist who specializes in pelvic health:
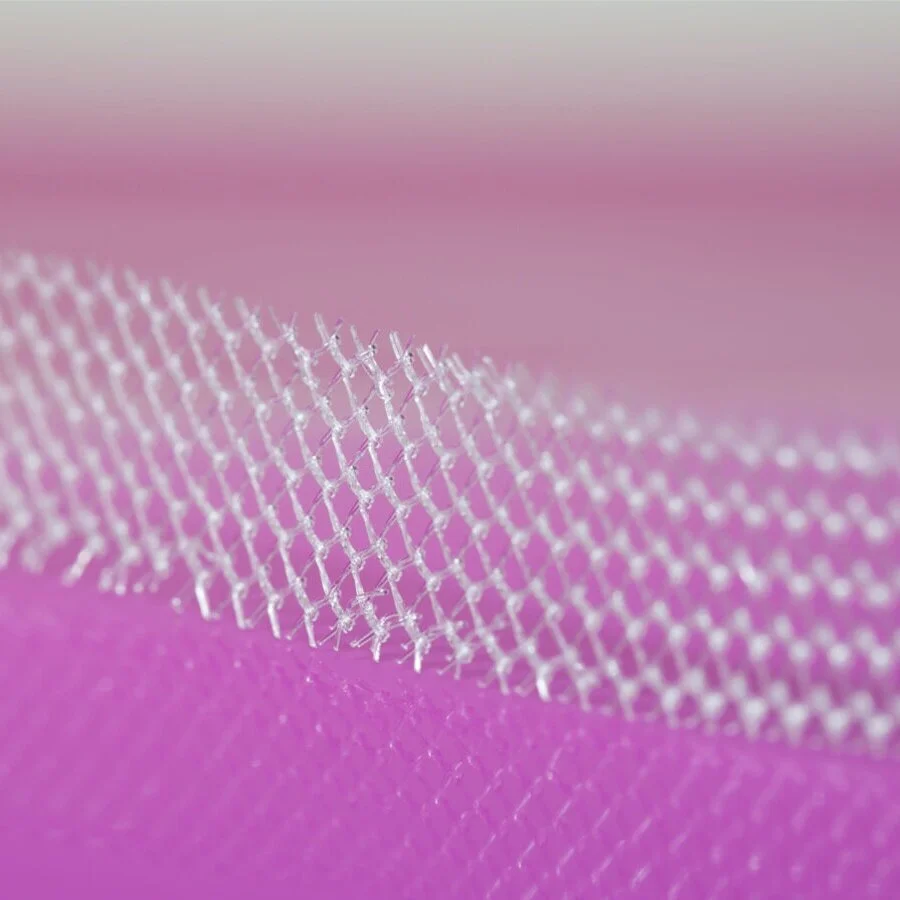
Your symptoms started after an incontinence surgery such as a mid-urethral sling
Your symptoms follow a vaginal prolapse repair with synthetic mesh
You have trouble emptying your bladder
You have a neurologic disease such as multiple sclerosis, spina bifida, or Parkinson disease
You previously have had treatment with pelvic radiation
Your symptoms started soon after a hysterectomy
Your bladder symptoms are accompanied by Urinary Tract Infections (UTI) three or more times a year or twice in 6 months.
What happens if I have Overactive Bladder symptoms and blood in my urine?
If you have blood in your urine that you can see, whether or not you have any other symptom, and no signs of a urinary tract infection, you should be evaluated by a urologist. We will often evaluate your kidneys with a CT scan as well as take a good look in your bladder with small scope called a cystoscope.
Blood in your urine that can only seen with a microscope sometimes does not require as extensive of an evaluation. Depending on your age, the amount of blood that was seen under the microscope, and your risk factors such as smoking and family history, we may recommend several different options. These can range from simply repeating a urine test in 6 months to a more extensive evaluation with a kidney ultrasound or a kidney CT and looking into your bladder with a scope.
Mid-Urethral Sling
What are the concerns about OAB symptoms if I had an incontinence sling?
If you have Overactive Bladder (OAB) symptoms and have had a previous incontinence sling such as a synthetic mid-urethral sling, this could be a warning sign. It is reassuring to note that most patients with OAB symptoms, even those who have a history of an incontinence sling, are just like any other OAB patient and will respond to the same types of therapy. The concern is that a small portion of people (perhaps 1-3%) who have synthetic slings will have some amount of blockage (obstruction) of their bladder from the sling. This is a small number, but it has to be considered as a possible cause if you have OAB symptoms after sling surgery. Common symptoms of an obstructing sling such as frequent and urgent urination or urgency incontinence, can be very similar to symptoms of OAB. It can even be difficult to determine if someone who had a previous sling surgery is suffering from OAB or symptoms of an obstructing sling. Slings can also, rarely, be placed so that a portion of them is through the bladder. This may also cause symptoms similar to Overactive Bladder.
If your OAB symptoms started long before or long after your sling surgery and you have no other bladder warning signs including trouble emptying your bladder, I think it is very reasonable to start out by approaching your Overactive Bladder treatment in the standard way. If you fail to see any improvement with multiple treatments or if you develop any new problems with treatment, I would then recommend a more thorough evaluation. But, if your OAB symptoms began shortly after placement of the sling, it could suggest that the sling surgery is related to your symptoms and you may need to see a bladder specialist.
I have OAB symptoms but it also feels like I’m not emptying my bladder?
It is very common for patients that I see with Overactive Bladder (OAB) to report that they feel like they do not empty their bladders all the way. If I urinated every 30 minutes (as some of my OAB patients do) I too would think I wasn’t emptying very well. Overactive Bladder can make you feel as though your bladder is still full even if you just urinated normally. But most of those patients do empty completely, they just feel as if they don’t. We can check how well patients empty with a test of the “post-void residual” (PVR), which is the amount of urine left in your bladder after you are done urinating. This is checked by either scanning the bladder with a portable ultrasound machine or (more rarely) placing a small catheter into the bladder to see how much is left behind. It can be important to evaluate this as some OAB medications can worsen problems with emptying your bladder.
If we find that you are one of those patients who really are not emptying their bladder, treatment for your symptoms can change significantly. As noted, OAB medications can make it even more difficult to empty so they may be avoided if you are already having trouble. Incomplete bladder emptying or urinary retention can be a cause of urinary frequency, urgency and incontinence. You will need a more thorough investigation of these symptoms if you are having urinary retention often including a pressure test of your bladder and possibly looking into your bladder with a cystoscope.
What if I have Overactive Bladder symptoms and urinary tract infections?
It is not unusual for me to see patients who have both Overactive Bladder and a history of recurrent urinary tract infections (UTI). I suspect this is because both are so common though it may also be because urinary incontinence is actually a risk factor for UTI. I always ask if the bladder symptoms completely go away when the infections are treated. If they respond I generally recommend that we get the infections under control before starting treatment for Overactive Bladder. This is because the symptoms may resolve completely once the infections are stopped.
Bladder Bacteria
However, it is also common for patients to report that the OAB symptoms started before the infections and do not go away with treatment of the infections. In these patients, it can make sense to begin treating the Overactive Bladder at the same time, especially if we suspect that urine leakage is increasing the risk of the UTI.
Urinary Tract Infections (UTI) that occur three or more times per year or twice in 6 months or that seem to very rapidly recur are called recurrent UTI. These may indicate the need further investigation. The evaluation may be as simple as an office visit and simple office tests. However, if you have a more complicated history such as previous pelvic surgery or trouble emptying your bladder, it may be appropriate to conduct a more thorough evaluation.
How is treating Overactive Bladder symptoms different in patients who have a neurologic disorder?
Treating OAB symptoms in patients with neurologic diseases such as multiple sclerosis, Parkinson disease, diabetic neuropathy or stroke is, in many ways, very similar to our approach in people without a neurologic issue with their bladder. We often start with behavioral therapies and frequently will add medications if symptoms are more bothersome. Even third-line therapies such as botulinum toxin injections and neuromodulation are used in patients with neurologic effects on the bladder, though the responses may be different. Also, we more commonly have to use higher doses of botulinum toxin in patients with neurologic issues than we do with OAB. While it depends on the neurologic disease, some patients with neurogenic bladder dysfunction are at higher risk for complications including not emptying the bladder (urinary retention), urinary tract infection, or damage to the kidneys. Patients with bladder symptoms from neurogenic bladder may also be harder to treat and less likely to respond to therapy. Patients with neurogenic bladder should probably be followed by a urologist, perhaps even one who specializes in bladder health, if available in your region.
Should I Worry?
I certainly do not mean to alarm anyone with this discussion of bladder warning signs. Warning in this case just means: Be careful. Most patients with OAB symptoms have none of these concerns. Even those that do are still more likely to have simple, uncomplicated OAB. However, enough patients with one or more of these warnings signs will have an underlying problem that it is worth meeting with an expert just to be sure that everything is all right.